Head Trauma Strongly Linked To Chronic Traumatic Encephalopathy But Precise Relationship Not Yet Known
Risk factors
Just as some athletes sustain concussion and others do not – despite experiencing blows to the head of similar magnitude and number – there is increasing evidence in the research to support the view that an accumulation of undiagnosed subconcussive head trauma and/or history concussive injury may lead to (or is the leading risk factor) for CTE. While a 2015 study (68) found that a history of concussive injury was the only risk factor consistently associated with CTE, “the apparent low incidence of CTE makes it challenging to draw definite conclusions on the condition’s risk factors.” (67) In other words, all neuropathologically confirmed cases of CTE involved individuals with a history of brain trauma exposure, but clearly not all individuals exposed to brain trauma develop CTE. (3, 67)
Among the other factors which, research suggests, may increase the risk of CTE besides repetitive head impacts include :
Genetic predisposition: It has been suggested that an important risk factor for CTE may be genetic predisposition, with preliminary studies linking the apolipoprotein E (APOE) gene to worse cognitive functioning in boxers and professional football players, and to prolonged recovery after a single traumatic brain injury. (13,14) A 2015 systematic review of all reported cases of CTE (68), however, found that there was no evidence to link genetic factors such as APOE to increased risk of CTE.
Few severe TBI versus many subconcussive blows: It is unknown if CTE is any more likely to manifest after a few severe traumatic brain injuries (TBIs) versus numerous repetitive subconcussive impacts (although a growing number of scientists appear to be leaning more towards the cumulative effect of subconcussive impacts as a cause);
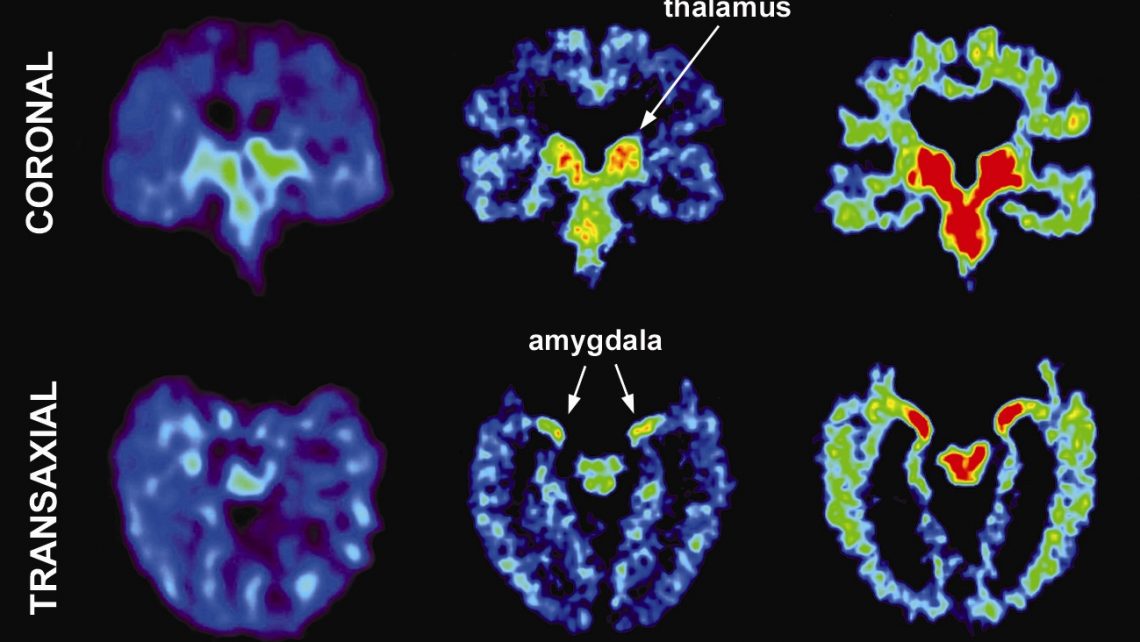
Number of hits: a 2014 study (55) found that the number of head impacts was related to substantive neurophysiological changes during the course of a football season, with all players sustaining more than 500 cumulative head impacts “flagged” for scoring more poorly on at least one component of the ImPACT neurocognitive test compared to their baseline, and/or displaying a statistically significant difference between pre- and post-season fMRI scans on 11 or more of 116 “regions of interest” in the brain.
A 2015 study found that high school players who sustained more than 900 hits over the course of a season were much more likely than players hit less than 600 times in a season to be flagged by ImPACT, fMRI, or both (57)
A 2014 study (64) reporting changes in brain white matter in a small group of college football players which persisted six months after the season was over found a strong correlation between changes to the white matter of the brain and the number of head hits with a peak rotational acceleration exceeding 4500 rad/sec2 and the number of head hits with a peak rotational acceleration exceeding 6,000 rad/sec2, and an especially strong correlation where the number of the former exceeded 30-40 for the season, and the number of the latter exceeded 10-15 for the season. (For reference, a person nodding his head up and down as fast as possible produces a rotational acceleration of approximately 180 rads/sec2).
Another 2015 study found that high school players who averaged more than 50 head impacts per week (coincidentally, the typical number of plays a high school football offense or defense runs in a game) were flagged at a rate of 83% while those who received less than 50 hits per week were only flagged 43% of the time, a threshold the researchers considered significant. (57)
Types and location of hits: Further complications in identifying risk factors arise when comparing impact exposure and type, both between and within sports. A 2010 study of college football players (6), for instance, found that head-impact exposure differed significantly by position, with linemen (both offensive and defensive) and linebackers receiving more impacts per practice and games than other positions, while linemen, linebackers and defensive backs received more impacts to the front of the head than the back, and quarterbacks experienced a higher percentage of impacts to the back of the head compared with the front. A 2015 study found that where on the helmet a player was hit most, rather than the absolute number of hits, was the best predictor of changes in the brain, suggesting that a player’s style of play may be particularly important in determining brain changes resulting from subconcussive impacts. (58)
Force of hits: A 2015 study found that high magnitude hits (over 60 g’s of linear force) players accrued over the course of a season were more likely to prompt abnormal biochemical/metabolic responses in regions of the brain responsible for executive and motor function. (56)
Age: Age at the time of injury may also affect an individual’s risk of developing CTE later in life, although the relationship is not understood. Because the developing brain is more “plastic” than the mature brain (e.g. has more ability to form new neural pathways to transmit information), it was originally thought that younger age at the time of mTBI had a beneficial effect on recovery and expected outcome, allowing a younger athlete to better compensate and recover after brain injury. Current literature, however, suggests that this is not the case; that the developing brain may actually be more susceptible and vulnerable to diffuse brain injury, which leads to more pronounced and prolonged cognitive deficits and hyperactivity. (7,8) “Therefore, it is possible that exposure to repetitive brain trauma at an early age may increase the risk of CTE more than exposure later in life, although this has yet to be proven.” (9)
Two 2015 studies (65, 66) suggest that beginning tackle football at an early age may increase the risk of cognitive problems later in life.
The first found that former NFL players who started playing tackle football prior to age 12 had approximately three times greater odds of having later-life, clinically-meaningful depression and executive dysfunction than those who started after age 12. (65) The second found that their brains displayed more changes to the microstructure of the corpus callosum, the bundle of neural fibers connecting the right and left hemispheres of the brain (66), which researchers theorized was the result of RHI disrupting, during a “window of vulnerability” between ages 10 and 12, the normal process of myelination (e.g. the development of myelin, an insulating layer or sheath that forms around nerves in the developing brain and spinal cord of the brain to allow electrical impulses to transmit quickly and efficiently along the nerve cells).
The findings of the two studies, however, was met with criticism from some head injury researchers as methodologically flawed (74-76), and a more recent study (71) was unable to replicate their findings. Studying data collected from another group of former NFL players, researchers could find no link between exposure to RHI in tackle football before high school and later life cognitive impairment, with the only statistically significant association being between learning disability and lower neurocognitive scores, not years of exposure to pre-high school football. (As a side note, unlike the previous studies, the new study received virtually no media attention, most likely because it didn’t fit neatly into the prevailing media’s narrative)
Gender. Girls and women appear to be at greater risk for concussion, and post-concussion syndrome-related symptoms (although a 2012 study (10) suggest that gender may not put girls at increased risk as earlier studies had suggested). Whether this puts them at greater risk of CTE is unknown.
Other health-related variables. Chronic inflammation associated with obesity, hypertension, diabetes, and heart disease may exacerbate neurodegeneration. A systematic review of all reported cases of CTE published in 2015 (68), however, found no evidence to link substance abuse or other pre-existing conditions to increased risk of CTE. A 2017 study (
Because scientists recognize that the study of CTE is in its infancy (3,14,16,68,70), many critical questions remain, among them: “how much brain trauma is causative, what type, and how frequent, the age when players are most susceptible and whether some individuals are genetically more prone than others.”
As Dr. Robert Stern of the CTE Center at Boston University told the CBS News magazine “60 Minutes” in November 2015 (70), “We know from all the neuropathologically confirmed cases of CTE that every case has had one thing in common, a history of repetitive head impacts. That means that… [i]t’s not good for you. It’s a necessary variable to get this disease. But just because you hit your head a bunch, doesn’t mean you’ll get the disease. So we have to figure out why one person gets it and another person doesn’t.”
The evidence, as Dr. McKee states in a 2012 CTE study (13), “clearly shows that, for some athletes and war fighters, there may be severe and devastating long-term consequences of repetitive brain trauma that has traditionally been considered only mild.”